Blood sugar usually returns to normal soon after delivery in gestational diabetes. But if you’ve had gestational diabetes, you’re at risk for future type 2 diabetes. You’ll continue working with your health care team to monitor and manage your blood sugar.
Causes
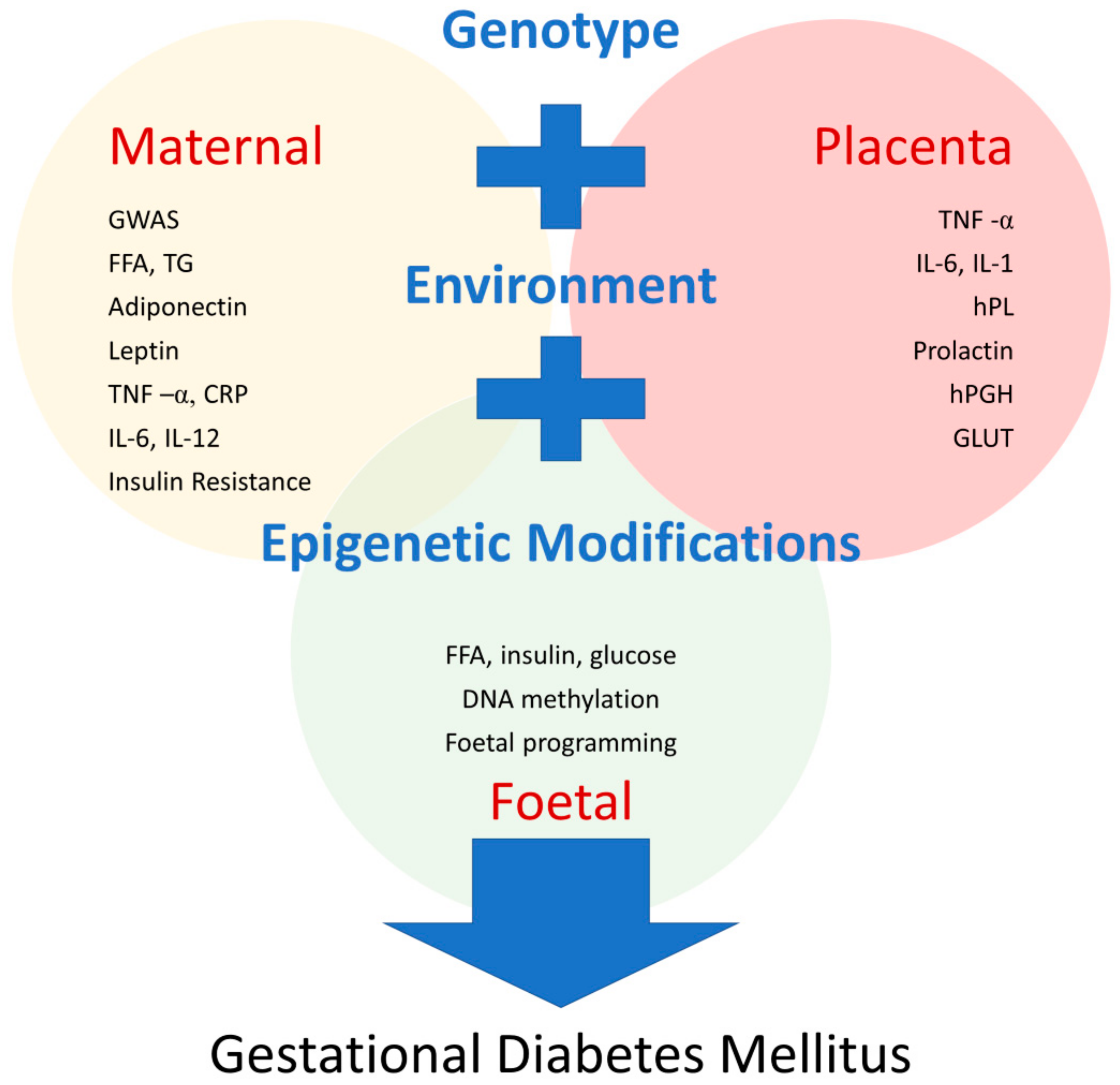
It is not known how and why some women develop gestational diabetes. To understand how gestational diabetes occurs, it can help to understand how pregnancy affects your body’s normal processing of glucose.
The food eaten is digested by the body to produce sugar (glucose) that enters your bloodstream. In response, your pancreas — a large gland behind your stomach — produces insulin. Insulin is a hormone that helps glucose move from your bloodstream into your body’s cells, where it’s used as energy.
The placenta that connects your growing baby to your blood supply produces high levels of various other hormones during pregnancy. Almost all of them impair the action of insulin in your cells, raising your blood sugar. Modest elevation of blood sugar after meals is normal during pregnancy.
The placenta produces more and more insulin-blocking hormones as your baby grows. In gestational diabetes, the placental hormones provoke a rise in blood sugar to a level that can affect the growth and welfare of your baby. Gestational diabetes usually develops during the last half of pregnancy — sometimes as early as the 20th week, but usually not until later.
Risk factors
Gestational diabetes can develop in any female, but some women are at greater risk. Risk factors for gestational diabetes include:
- 1. Greater than 25 age. Women older than age 25 are more likely to develop gestational diabetes.
- 2. Personal or family health history. Your risk of developing gestational diabetes increases if you have prediabetes — slightly elevated blood sugar that may be a precursor to type 2 diabetes — or if a close family member, such as a parent or sibling, has type 2 diabetes. You’re also more likely to develop gestational diabetes if you had it during a previous pregnancy, if you delivered a baby who weighed more than 9 pounds (4.1 kilograms), or if you had an unexplained stillbirth.
- 3. Being overweight. You’re more likely to develop gestational diabetes if you’re significantly overweight with a body mass index (BMI) of 30 or higher.
- 4 .Racial factors. For reasons that aren’t clear, women who are black, Hispanic, American Indian or Asian are more likely to develop gestational diabetes.
Symptoms
Gestational diabetes, for most women, doesn’t cause noticeable signs or symptoms. Rarely, gestational diabetes may cause excessive thirst or increased urination.
Seek health care early, if possible, when you first think about trying to get pregnant — so your doctor can evaluate your risk of gestational diabetes as part of your overall childbearing wellness plan. Once you become pregnant, your doctor will address gestational diabetes as part of your regular prenatal care. If you develop gestational diabetes, you may need more frequent checkups. These are most likely to occur during the last three months of pregnancy when your doctor will carefully monitor your blood sugar level and your baby’s health.
You may be referred to additional health professionals who specialize in diabetes management, such as an endocrinologist, a registered dietitian or a diabetes educator. They can help you learn to manage your blood sugar level during your pregnancy.
Your health care team will check your blood sugar right after delivery and again in six weeks to make sure that your blood sugar level has returned to normal after your baby is born. Once you’ve had gestational diabetes, it’s a good idea to have your blood sugar level tested regularly. The frequency of blood sugar tests will in part depend on your test results soon after you deliver your baby.
Diagnosis
There is no single set of screening guidelines for gestational diabetes. Some question whether gestational diabetes screening is needed if you’re younger than 25 and have no risk factors. Others say that screening all pregnant women — no matter their age — is the best way to catch all cases of gestational diabetes.
When to screen
Evaluation of your risk factors by your doctor will happen for gestational diabetes early in your pregnancy.
In case of a higher risk— for example, your body mass index (BMI) before pregnancy was 30 or higher or you have a mother, father, sibling or child with diabetes — your doctor may test for diabetes at your first prenatal visit.
You’ll likely have a screening test for gestational diabetes sometime during your second trimester — between 24 and 28 weeks of pregnancy if you’re at average risk of gestational diabetes.
Routine screening for gestational diabetes
Glucose challenge test (initial). This test begins by drinking a syrupy glucose solution. One hour later, you’ll have a blood test to measure your blood sugar level. A blood sugar level below 130 to 140 milligrams per deciliter (mg/dL), or 7.2 to 7.8 millimoles per liter (mmol/L), is usually considered normal on a glucose challenge test, although this may vary at specific clinics or labs. If your blood sugar level is higher than normal, it only means you have a higher risk of gestational diabetes. Your doctor will diagnose you after giving you a follow-up test.
Glucose tolerance testing (follow up). You’ll be asked to fast overnight for the follow-up test and then have your fasting blood sugar level measured. Then you’ll drink another sweet solution — this one containing a higher concentration of glucose — and your blood sugar level will be checked every hour for a period of three hours. If at least two of the blood sugar readings are higher than normal, you’ll be diagnosed with gestational diabetes.
If you’re diagnosed with gestational diabetes
Your doctor will likely recommend frequent check-ups if you have gestational diabetes, especially during your last three months of pregnancy. During these exams, your doctor will carefully monitor your blood sugar. Your doctor may also ask you to monitor your own blood sugar daily as part of your treatment plan.
You may need additional tests to evaluate your baby’s general health if you’re having trouble controlling your blood sugar, or you need to take insulin, or you have other pregnancy complications. These tests assess the function of the placenta, the organ that delivers oxygen and nutrients to your baby by connecting the baby’s blood supply to yours. If your gestational diabetes is difficult to control, it may affect the placenta and endanger the delivery of oxygen and nutrients to the baby. Tests to monitor your baby’s well-being include:
- 1. Nonstress test. In this test sensors are placed on your stomach and connected to a monitor to measure your baby’s heart rate, which should increase when the baby moves. If your baby’s heart doesn’t beat faster during movement, the baby may not be getting enough oxygen.
- 2. A biophysical profile (BPP). A combination of a nonstress test with an ultrasound study of your baby in called BPP. There’s a scoring system that enables your doctor to evaluate your baby’s heartbeat, movements, breathing and overall muscle tone, and determine whether your baby is surrounded by a normal amount of amniotic fluid. Your baby’s scores on heartbeat, breathing, and movement help your doctor tell if the baby’s getting enough oxygen. When the amniotic fluid is low, it may mean that your baby hasn’t been urinating enough. This could indicate that over time the placenta has not been working as well as it should.
- 3. Fetal movement counting. This is a simple test performed at the same time as the nonstress test or the biophysical profile. You simply count how often your baby kicks over a set time. The infrequent movement may mean your baby isn’t getting enough oxygen.
Treatment
Monitor and control your blood sugar to keep your baby healthy and avoid complications during your pregnancy and delivery. Also, keep a close eye on your future blood sugar levels. Management strategies may include:
- 1. Blood sugar monitoring. Your health care team may ask you to check your blood sugar four to five times a day while you’re pregnant — first thing in the morning and after meals — to make sure your level stays within a healthy range. This may sound inconvenient and difficult, but it’ll get easier with practice.
- 2. Blood sugar monitoring will also be done during labor and delivery. Follow-up blood sugar checks are also important. After having gestational diabetes, you’re at increased risk of later developing type 2 diabetes. Work with your health care team to keep an eye on your levels. Maintaining health-promoting lifestyle habits, such as a healthy diet and regular exercise, can help reduce your risk.
- 3. Healthy diet. The best way to control blood sugar is to eat the right kinds and quantity of food. Doctors don’t advise losing weight during pregnancy — your body is working hard to support your growing baby. But your doctor can help you set weight gain goals based on your weight before pregnancy. Making healthy food choices can help prevent excessive weight gain, which can put you at higher risk for complications.