PCOS cause is unknown but early diagnosis and treatment may reduce the risk of long-term complications, such as type 2 diabetes and heart disease.
Each month several follicles start to develop, but normally just one fully develops and goes on to ovulate. The name PCOS comes from the appearance of the ovaries in most, but not all, women with the disorder — enlarged and containing numerous small cysts located along the outer edge of each ovary (polycystic appearance).
Causes
Although the exact cause is not totally clear, several factors probably play a part. These include the following:
- Insulin. Insulin resistance is present in women with PCOS. This means that cells in the body are resistant to the effect of a normal level of insulin. More insulin is produced to keep the blood sugar normal. This raised level of insulin in the bloodstream is thought to be the main underlying reason why PCOS develops. It causes the ovaries to make too much testosterone. A high level of insulin and testosterone interfere with the normal development of follicles in the ovaries. As a result, many follicles tend to develop but often do not develop fully. This causes problems with ovulation: hence period problems and reduced fertility. The increased testosterone level in the blood causes excess hair growth on the body and thinning of the scalp hair. Increased insulin also contributes towards weight gain.
- Luteinising hormone (LH). This hormone, manufactured in pituitary gland, stimulates the ovaries to ovulate and works alongside insulin to promote testosterone production. A high level of LH is found in about 4 in 10 women with PCOS. A high LH level combined with a high insulin level means that the ovaries are likely to produce too much testosterone.
Hereditary factors. A patient’s genetic makeup makes her more prone to developing PCOS. PCOS is not strictly inherited from parents to children, but it may run in some families.
Weight. Although being overweight or obese is not the underlying cause of PCOS, it makes insulin resistance worse. This may then cause the level of insulin to rise even further. High levels of insulin can contribute to further weight gain producing a ‘vicious cycle’. Losing weight, although difficult, can help break this cycle.
Symptoms
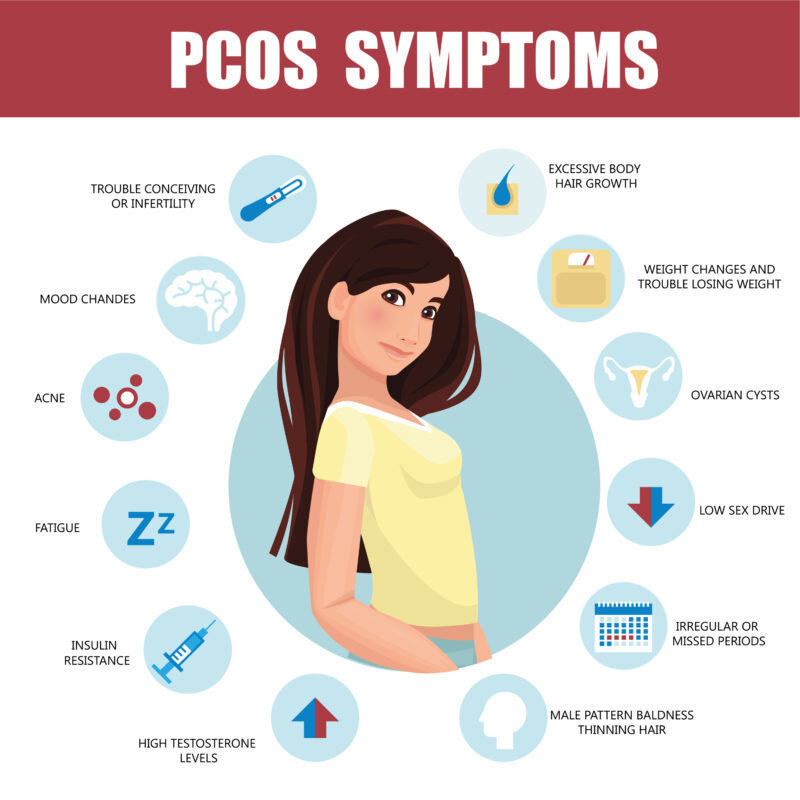
Symptoms that occur if you do not ovulate
- Problem with periods occur in about 7 in 10 women with PCOS. You may have irregular or light periods, or no periods at all.
- Problems with fertility may occur. A female needs to ovulate to become pregnant. She may not ovulate each month, and some women with PCOS do not ovulate at all. PCOS is one of the most common causes of infertility.
Symptoms that can occur if you make too much testosterone (male hormone)
- Hair growth (hirsutes) in excess occurs in more than half of women with PCOS. It is mainly on the face, lower abdomen, and chest. This is the only symptom in some cases.
- Persistence of acne may persist beyond the normal teenage years.
- Scalp hair thinning (similar to male pattern baldness) occurs in some cases .
Other symptoms
- Gain in weight gain – about 4 in 10 women with PCOS become overweight or obese.
- Symptoms of depression or poor self-esteem may develop as a result of the other symptoms.
Typical symptoms originate in the late teens or early 20s. Not all symptoms occur in all women with PCOS. For example, some women with PCOS have some excess hair growth, but have normal periods and fertility.
Severity of symptoms can vary from mild to severe. Mild unwanted hair, for example, is normal, and it can be difficult to say when it becomes abnormal in women with mild PCOS. At the other extreme, women with severe PCOS can have marked hair growth, infertility, and obesity. Symptoms may also change over the years. For example, acne may become less of a problem in middle age, but hair growth may become more noticeable.
Diagnosis
The diagnosis of PCOS is one of exclusion as there’s no specific test to definitively diagnose polycystic ovary syndrome. The doctor considers all of your signs and symptoms and then rules out other possible disorders. Your doctor takes many factors into account during this process:
- Past medical history. Questions may be asked about your menstrual periods, weight changes and other symptoms.
- Complete physical examination. Your doctor will note several key pieces of information, including your height, weight and blood pressure during your physical exam.
- Pelvic examination. Your doctor visually and manually inspects your reproductive organs for signs of masses, growths or other abnormalities during a pelvic exam.
- Blood tests. Doctor may ask for blood to be drawn to measure the levels of several hormones to exclude possible causes of menstrual abnormalities or androgen excess that mimic PCOS. Additional blood testing may include fasting cholesterol and triglyceride levels and a glucose tolerance test, in which glucose levels are measured while fasting and after drinking a glucose-containing beverage.
- Pelvic ultrasound. Ultrasound of the pelvis may show the appearance of your ovaries and the thickness of the lining of your uterus. During the test, you lie on a bed or examining table while a wand-like device (transducer) is placed in your vagina (transvaginal ultrasound). The transducer emits inaudible sound waves that are translated into images on a computer screen.
Complications
Suffering from PCOS increases the likelihood of following conditions, especially if obesity also is a factor:
- Raised blood pressure
- Cholesterol and lipid abnormalities, such as elevated triglycerides or low high-density lipoprotein (HDL) cholesterol, the “good” cholesterol
- Type 2 diabetes
- Increased levels of C-reactive protein, a cardiovascular disease marker
- Metabolic syndrome, a cluster of signs and symptoms that indicate a significantly increased risk of cardiovascular disease
- Nonalcoholic steatohepatitis, a severe liver inflammation caused by fat accumulation in the liver
- Sleep apnea
- Abnormal uterine bleeding
- Cancer of the uterine lining (endometrial cancer), caused by exposure to continuous high levels of estrogen
- Gestational diabetes or pregnancy-induced high blood pressure, if you do become pregnant
Treatment
- Treatment of polycystic ovary syndrome generally focuses on management of your individual main concerns, such as infertility, hirsutism, acne or obesity.
Surgery
An outpatient surgery called laparoscopic ovarian drilling is an option for some women with PCOS if medications don’t help you become pregnant. Your doctor can help you determine if you’re a candidate for this type of surgery.
A surgeon makes a small incision in your abdomen and inserts a tube attached to a tiny camera (laparoscope) in this procedure. The camera provides the surgeon with detailed images of your ovaries and neighboring pelvic organs. The surgeon then inserts surgical instruments through other small incisions and uses electrical or laser energy to burn holes in follicles on the surface of the ovaries. The goal is to induce ovulation.
Prevention
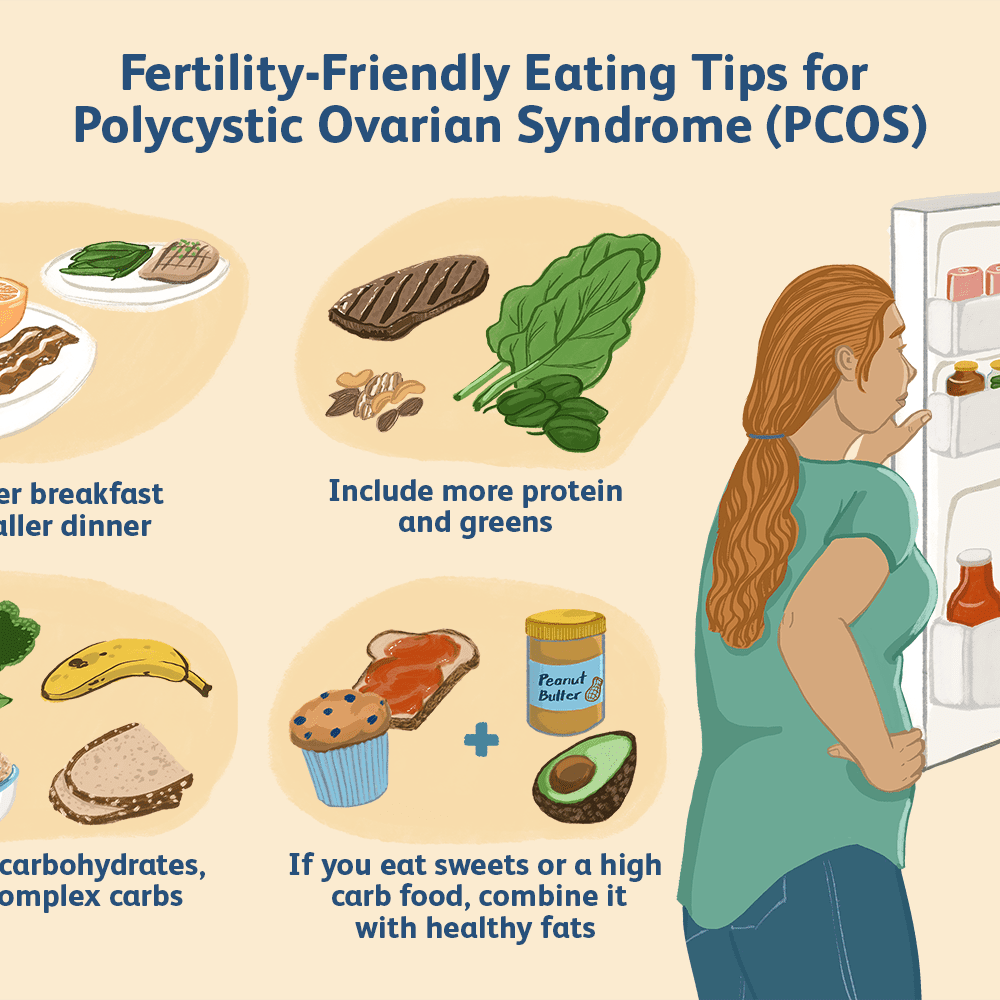
Effects of PCOS can be offset by paying attention to the foods you eat and your activity levels:
- Maintain optimum weight. Obesity makes insulin resistance worse. Weight loss can reduce both insulin and androgen levels, and may restore ovulation. No single specific dietary approach is best, but losing weight by reducing total calorie intake can benefit the overall health of women with polycystic ovary syndrome. Ask your doctor to recommend a weight-control program, and meet regularly with a dietitian for help in reaching weight-loss goals.।
- Improve dietary habits. Low-fat, high-carbohydrate diets may increase insulin levels, so you may want to consider a low-carbohydrate diet if you have PCOS — and if your doctor recommends it. Don’t severely restrict carbohydrates; instead, choose complex carbohydrates, which are high in fiber. The more fiber in a food, the more slowly it’s digested and the more slowly your blood sugar levels rise. High-fiber carbohydrates include whole-grain breads and cereals, whole-wheat pasta, bulgur, barley, brown rice, and beans. Limit less healthy, simple carbohydrates such as soda, excess fruit juice, cake, candy, ice cream, pies, cookies and doughnuts.
- Increase activity level. Exercise helps lower blood sugar levels. If you have PCOS, increasing your daily activity and participating in a regular exercise program may treat or even prevent insulin resistance and help you keep your weight under control.